When looking into healthcare sharing after only having health insurance, you may wonder how the members’ medical bills are being taken care of.
Let’s first take a look at how claims are paid through traditional health insurance.
Essentially, health insurance subscribers enter into an arrangement with a health insurance company in order to reduce the impact of the cost of medical expenses. There are many different types of insurance coverage plans with even more ways of paying for them.
A co-insurance is a type of arrangement with the insurance company that divides the responsibility for payment by a percentage. Co-insurances are listed with the insurance company portion listed first, and then the subscribers.
Sharing ministries and not-for-profit organizations do not use insurance terminology, but do have program equivalents.
Just like insurance, there is a portion that you are responsible for paying before your bill sharing plan kicks in. Insurance companies call this your deductible amount. Deductible = Personal Responsibility Amount (PRA), an annual household portion (AHP), or Annual Unshared Amount (AUA).
The monthly amount you pay for your health insurance is called your Premium. Healthcare Sharing ministries and not-for-profits typically call this your Monthly Share.
An insurance claim is a request for payment that you or your health care provider submits to your health insurer when you get items or services you think should be covered. Members of Impact do not file claims because Impact Health Sharing is not an insurance company. Sharing ministries and not-for-profit organizations typically call these an eligible event, incident, or illness.
EOB stands for Explanation of Benefits. This is a document an insurance company sends you to inform you that a claim has been processed. Healthcare Sharing ministries and not-for-profit organizations usually call these an Explanation of Sharing (EOS). The EOS will show you what has been shared and what amount you may still be responsible for.
What happens when you go to a provider?
Impact Health Sharing members present their member ID cards to their service providers. The service provider then discounts the bill accordingly. The bill is then sent to us. Here, we review the services provided to determine if the bill is eligible for sharing. After the PRA has been met and if the bill is eligible, it is then shared among the other members.
Always review your Explanation of Sharing (EOS) and compare it to the bill from your provider for your portion. If the amounts match, then you will be responsible for paying that portion. If the amounts do not match, please call Impact so that we can help.
Reference Based Repricing ensures fair and just pricing for all claims. Our approach includes three key components to ensure claims are priced fairly for everyone involved.
First, we audit each claim using our industry-leading Medical Bill Review program. This helps us identify any inaccuracies or inconsistencies in the billing process. Next, we determine the "best price" for each claim using multiple methodologies and 15 years of claims history. This includes utilizing historical data, reference-based benchmarks, direct contracts, fair market value, and fee-for-service pricing.
Finally, we determine what is considered fair-marketing pricing for the services rendered.
98% of the time, the provider accepts the initial payment from Impact Health Sharing. However, we know that some providers have billing systems configured to automatically generate balance bills to patients if they receive a payment for less than the initial billed charges. If this happens, it's important that our members call us right away. Once we have been notified, we will work directly with the provider to settle the account through further negotiation.
At Impact Health Sharing, we are committed to providing fair and just pricing for all of our members. We believe that by utilizing our Reference Based Repricing process, we can ensure that employees receive the best possible care and have a positive member experience.
What is an Eligible Medical Bill?
An Eligible Medical Bill is an incurred medical bill, which meets the criteria for sharing as established in the Guidelines. The Eligible Medical Bill may be reduced by any discounts, fees, or other sources of payment.
What does Eligible for Sharing mean?
Eligible for Sharing refers to any testing, treatment, procedure, or service that meets the criteria for sharing as established in the Guidelines.
If you recently lost your health plan, or even if you signed up for another plan, you can join Impact Health Sharing and make a change for the better! Impact Health Sharing Works Better, Feels Better than insurance. Just ask one of the millions of Americans who are members of a Healthcare Sharing Organization and have found that this approach really does offset the rising costs of healthcare.
Impact Health Sharing delivers a modern and affordable alternative to health insurance. In a lot of ways, it acts the same as your current health plan, but it's different in the ways that matter most.
Our “love thy neighbor” approach takes a principle that has been in practice for centuries and adds modern technology to automate the process of allowing everyone to pay for one another's medical bills. Impact Health Sharing embraces the digital age and the reality that these advances disrupt the institutions of old. Simply put, Impact Health Sharing helps communities of families, individuals, and small businesses leverage social technology to share and pay one another's medical bills.
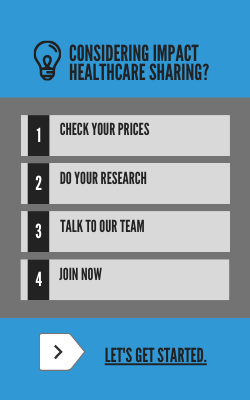
To start saving money, explore your options here.